Learning Outcomes
- Determine when to escalate to triple oral therapy and non-insulin injectable treatments
- Impact of other medical conditions and their treatments on glycaemic control
- Approach to managing blood glucose levels in patients wishing to lose weight
- Individualising glycaemic treatment targets depending on patient wishes, comorbidities and risk of hypoglycaemia
Visit One
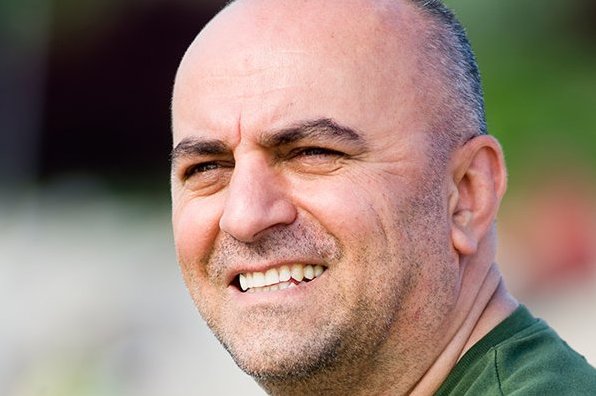
Antony is a 40-year old male diagnosed with type 2 diabetes, two years ago. Screening for complications is up to date with no evidence of micro- or macrovascular disease. Past medical history is significant for moderate persistent asthma since childhood. Antony often forgets to take his asthma preventative medications and consequently has frequent hospital admissions for exacerbations that require treatment with parental and oral corticosteroids. Weight has been a significant issue since adolescence and has further increased in the past six months following the introduction of sulfonylurea therapy. Antony is a chef in a fast food restaurant, working long hours with a poor diet of high fat foods. He consumes alcohol on social occasions. He participates in indoor cricket competitions with twice weekly training sessions and goes on long bike rides with friends on weekends. Antony states he is keen to address his diabetes and weight issues but will not consider restrictive/fad diets or surgical options. He is unwilling to consider injectable therapy at this stage.
Current medications
Metformin 500mg three times daily
Gliclazide MR 60mg daily
Pantoprazole 40mg daily
Fluticasone propionate 250µg + Salmerterol 50µg powder for inhalation twice daily
Salbutamol 100mcg MDI PRN
Allergies
Nil known drug allergies
Examination
Blood pressure 125/80 mmHg
Weight 94 kg, Height 170 cm, BMI 33 kg/m2
Abdominal adiposity, but nil evidence of Cushing’s syndrome
Ankle jerks present, monofilament sensation intact, pedal pulses present.
Nil evidence of foot ulceration
Investigations
HbA1c 68.3 mmol/mol (8.4%)
Urine albumin/ creatinine ratio (ACR) <2.5 mg/mmol
eGFR >90 ml/min/m2
What are the management issues for this patient?
- Optimising metformin dosage in patients with normal renal and hepatic function
- Individualising glycaemic treatment targets depending on patient wishes, co-morbidities and hypoglycaemia risk
- Escalation of glucose lowering therapy to triple oral and noninsulin injectable treatments
- Considerations when selecting third line agents with a view to minimising weight gain/aid weight loss
- Metformin and DPPIV inhibitors are weight neutral, Sulfonylurea agents are associated with modest weight gain, SGLT2 inhibitors and GLP1 analogues are associated with weight loss. Within each class, some agents may result in greater weight loss than others.
- The impact of comorbid conditions and their treatments on glycaemic control in type 2 diabetes
What is your management plan?
- Patient’s age and lack of medical co-morbidities suggest that an HbA1c target of 48 mmol/mol (6.5%) would be appropriate.
- Lifestyle modification- diet and exercise, dietician review.
- Continue gliclazide.
- Increase dose of metformin to an optimal dose of 2g per day, the extended release formulation may promote better adherence given once daily dosing.
- Start a SGLT2 inhibitor. Potential side effects are explained and advice provided regarding genitourinary hygiene to prevent genitourinary tract infection. The option a GLP-1RA may be considered for its weight reducing effect if the patient were willing to take injectable therapy.
- A combination formulation with extended release metformin and SGLT2 inhibitor may be considered to reduce tablet load and further promote medication adherence.
- Address asthma management plan, encourage adherence to preventative medications.
- Screen for other conditions contributing to obesity e.g. hypothyroidism.
Visit Two
Antony returns six months later for review. Lifestyle modification including weight loss of 5kg with the change in his medication has resulted in an improvement in glycaemic control; HbA1c is now 56 mmol/mol (7.3%). BGL monitoring indicates predominantly postprandial hyperglycaemia. Antony has not had any asthma symptoms or exacerbations and has been able to wean his preventer inhaler to a maintenance dose. He has had one episode of mild balanitis in the last six months. He has no history of pancreatitis.
Current medications
Dapagliflozin 5mg/ MetforminXR 1g 2 tablets daily
Gliclazide MR 60mg daily
Salbutamol 100mcg MDI PRN
Fluticasone propionate 250µg + Salmerterol 50µg powder for inhalation twice daily
Examination
Blood pressure 120/80 mmHg
Weight 89 kg, Height 170 cm, BMI 30 kg/m2
What are the management issues for this patient?
- Intensification of glucose lowering therapies
- Injectable, non-insulin therapy for diabetes
- Side effects of SGLT2 inhibitors
What is your management plan?
- Referral to community based lifestyle modification program for ongoing weight management.
- Continue Dapagliflozin 5mg/ Metformin XR 1g.
- Increase gliclazide MR to 120mg.
Alternative Plan
- Referral to community based lifestyle modification program for ongoing weight management.
- Cease SGLT2 inhibitor.
- Continue metformin XR 2g daily and gliclazide MR 60mg.
- Start GLP-1RA with breakfast. Potential side effects are explained (nausea, vomiting, pancreatitis).
- Referral to a diabetes nurse educator for education regarding administration of GLP-1RA injectable therapy.
Further Key Learnings
Mechanisms of action of glucose lowering therapies
- Metformin decreases hepatic glucose production, improves glucose clearance through an improvement of hepatic insulin sensitivity, Decreases fatty acid oxidation, and increases glucagon-like peptide 1 (GLP-1)
- Sulfonylurea agents inhibit pancreatic beta-cell ATP-sensitive potassium channels and enhance insulin secretion
- DPP-4 prevent the degradation of endogenous GLP-1, thereby prolonging its insulinotropic activity
- SGLT2 inhibitors inhibit the sodium-glucose cotransporter 2 (SGLT2) in the proximal renal tubules, reducing reabsorption of filtered glucose from the tubular lumen and lowering the renal threshold for glucose, resulting in increased urinary excretion of glucose, thereby reducing plasma glucose concentrations. It is not advised to use NSAIDs or loop diuretics (e.g. frusemide) with SGLT2 inhibitors as these medications can affect kidney filtration rates, increasing drug exposure, especially in the elderly or volume-depleted.
- GLP1 receptor agonists (GLP-1RA), are analogues of human GLP-1 and are administered by subcutaneous injection. They stimulate beta-cell insulin release and slow gastric emptying, which contributes to weight loss
- Insulin directly stimulates the insulin receptor
SGLT2 inhibitors and Diabetic Ketoacidosis
Diabetic ketoacidosis is a very rare but potentially serious side effect of SGLT2 inhibitors. Traditionally this occurs with consistently high blood glucose levels and is rare in type 2 diabetes but very occasionally it can occur with normal blood glucose levels when SGLT2 inhibitors are being taken.
Symptoms of diabetic ketoacidosis include:
- nausea and vomiting
- abdominal pain
- dehydration
- blurred vision
- fever
- sweet smell of ketones on breath
- difficulty breathing
SGLT2 inhibitors should be withheld temporarily when are not eating or drinking for an extended period of time and restart when well, e.g. fasting for surgery, unwell with an illness or unable to eat due to vomiting.
Additional Resources
Rosenstock J and Ferrannini E. Euglycemic Diabetic Ketoacidosis: A Predictable, Detectable, and Preventable Safety Concern with SGLT2 Inhibitors. Diabetes Care 2015; 38: 1638-1642